Introduction
The clinical practice of infectious diseases requires each human being to be versed on a multitude of healthcare basic issues that range from infection prevention, right diagnosis, and right treatment. The Clinical Practice section of this website or related work of SASPI offers help to healthcare professionals to increase their value in healthcare resulting in benefits to the whole society. These resources include tools and practical information on IAS practices and clinical quality performance improvement measurements.
Considering the importance of integrated antimicrobial stewardship (IAS) practices by each hospital and each healthcare worker (HCW), it is vital to have a practice statement from SASPI based on available evidence from the literature and a recently completed Delphi study under SASPI. This document is developed and finalized through a Delphi model where it was prepared by three Indian experts (An ID physician, A Pharmacologist and A Microbiologist) in the first phase, and shared with SASPI members with experts in the same field (at least one expert (HICC/AMSP member) from 31 tertiary care institutes/hospitals) for content validation and comments regarding the feasibility of their practices in the second phase, and lastly again verified by same three experts of the first phase and prepared the practice statements with consideration of all relevant comments by individual institute experts in third phase. These practice statements are the baseline Indian practice guidance towards IAS practices to curtail AMR in tertiary care hospitals. Each Indian hospital is advocated to follow these practices. With time, through multi-centric participation under the banner of SASPI, these practices will be monitored and updated towards higher goals.
IAS Practice Statements
Considering the importance of integrated antimicrobial stewardship (IAS) practices by each hospital and healthcare worker (HCW), it is vital to have a practice statement from SASPI based on available evidence from the literature and a recently completed Delphi study under its guidance. This document was developed and finalized through a Delphi process. In the first phase, it was prepared by three Indian experts (an ID physician, a pharmacologist, and a microbiologist). In the second phase, it was shared with SASPI members and experts from the same fields (with at least one expert from each of 31 tertiary care institutions/hospitals, including HICC/AMSP members) for content validation and feedback on the feasibility of the proposed practices. In the third phase, the document was reviewed and revised by the same three experts from the first phase, taking into account all relevant comments from the individual institute experts.
These practice statements serve as the baseline Indian practice guidelines for IAS practices in tertiary care hospitals to combat antimicrobial resistance (AMR). It is recommended that each Indian hospital adopt these practices. Over time, through multi-center collaboration under SASPI, these practices will be monitored and updated to achieve more ambitious goals.
Implementation of Antimicrobial Stewardship (IAS) Practices
Workflow Overview – Expert Video Session
Stewardship Pearls
This is a platform for sharing bedside or laboratory stories (text, image, video) on integrated antimicrobial stewardship activities in daily practices by both the general public and healthcare workers. These contributions aim to create better practice opportunities for everyone in infection prevention, accurate diagnosis, and responsible antimicrobial prescriptions—fostering a better world through a One-Health approach.
We invite anyone to share their own story, which will be published in each issue of JASPI following the editor’s review. Read more…
Kindly submit your stories using [this link].
Journal Autopsy
Journal Autopsy is your go-to resource for the latest and most influential updates in Integrated Antimicrobial Stewardship (IAS). Edited by Dr Sivanantham Krishnamoorthi and a dedicated editorial team, this section of JASPI brings you the critical insights and cutting-edge research you need to stay ahead in the evolving landscape of IAS.
For details information Click Here!
Practice-Changing Guidelines in Local Institutions
Pan-India representations
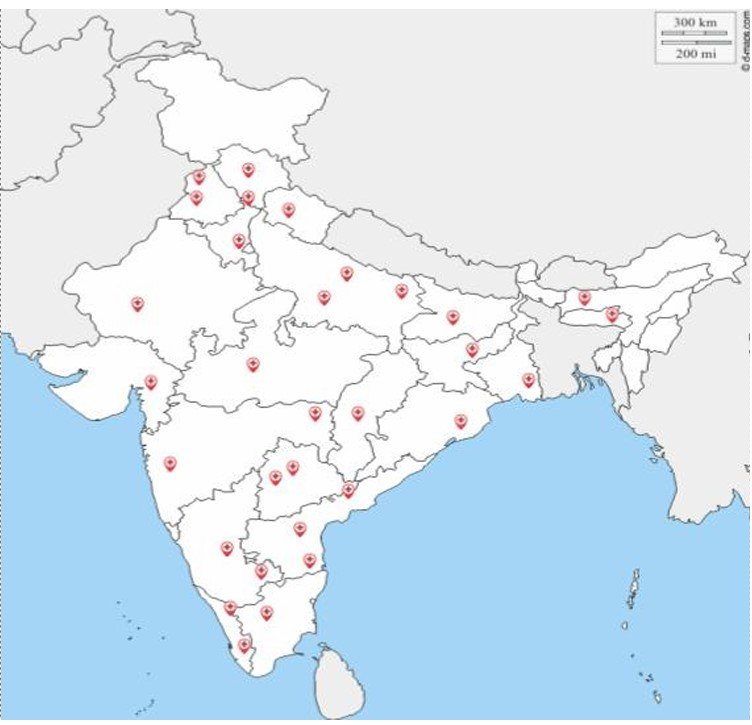
Institute List
- AIIMS, Nagpur
- AIIMS, Guwahati
- JIPMER, Puducherry
- SGPGIMS, Lucknow
- AIIMS, Raipur
- AIIMS, Patna
- AIIMS, Bilaspur
- AIIMS, Rishikesh
- AIIMS, Bathinda
- AIIMS, Jodhpur
- AIIMS, New Delhi
- AIIMS, Mangalagiri
- AIIMS, Deoghar
- AIIMS, Kalyani
- AIIMS, Madurai
- General Medicine, NEIGRIHMS
- AIIMS, Bibinagar
- AIIMS, Bhopal
- AIIMS, Gorakhpur
- AIIMS, Raebareli
- PGIMER, Chandigarh
- Sree Gokulam Medical College and Research Foundation
- Believers Church Medical College Hospital, Thiruvalla, Kerala





